Hearts Keep Drumming
Oh life
Is just a game
No one ever tells you how to play
See different people
Go different ways
Some of them will leave you but
Some of them will stay
Well our hearts keep drumming
And the years keep coming
Quicker than they’ve ever been
You’re sick of the same thing
But it’s quicker than changing
It’s too late to begin
Well everybody’s running
But you don’t know where
Time is running thin
Everybody’s looking for somebody to love
But we’re scared to let them in
And I say oh oh oh
Are there any survivors?
Am I here alone?
I say oh oh oh
Are there any survivors?
Am I here alone?
Am I on my own?
Am I on my own?
Oh love
It comes and goes
But no one never tells you how to learn to let go
Different people, they walk different roads
Some of them will hurt you but
Some of them won’t
Well the bridge is burning
And the wheel keeps turning
Quicker than it did before
Your heart screams “yes”
Your head says “no”
And you’re never really sure
Well everybody’s running
But you don’t know why
Time is running short
Everybody’s looking for a place to hide
So there’s no one left at all
Survivors
By Passenger
It’s been almost a year since I have posted on my blog. It’s not that I have not written, I just did not feel like sharing what I wrote, as it has been a difficult year and I have felt guarded. Everything I wrote just seemed so dark and depressing. I judge myself a lot harsher than I would anyone else and feel like what I have written is utter crap. This past year has felt like being on the biggest and craziest roller coaster at six flags. Not only have I had some of my lowest moments, I have also had some really good experiences, in which I have pushed myself out of my comfort zone. These experiences seem to have changed me in substantial ways and pushed me to grow in ways I don’t think I otherwise would have.
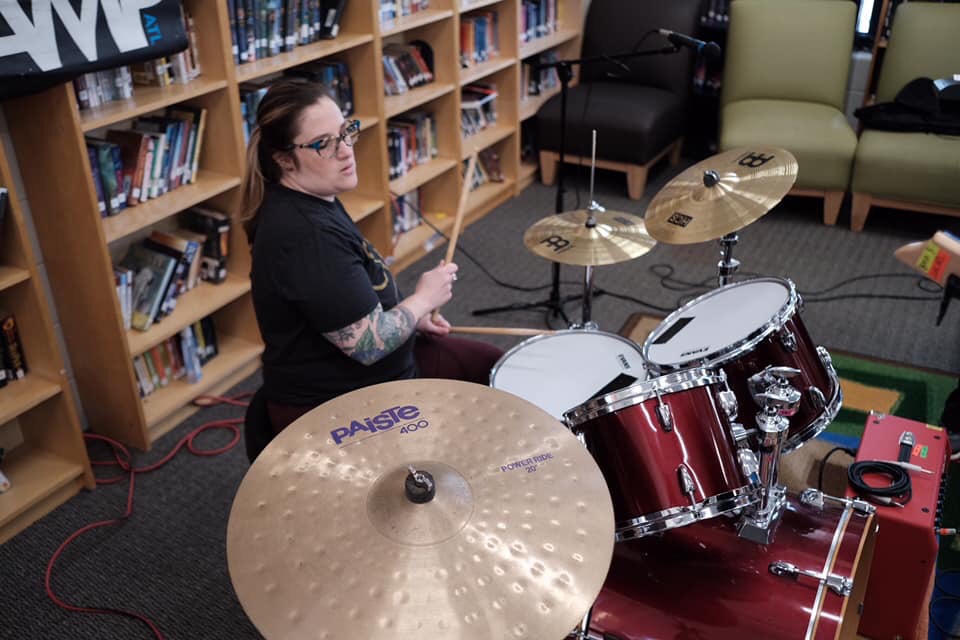
In February after years of hearing about it, I took part in Ladies Rock Camp. Thanks to my friend, Emily (!) and all my awesome friends who donated towards my tuition. This is basically a 3 day music camp for adults that includes music lessons, we are split into bands, and then tasked to write an original song and then perform it at a venue. I was so excited and nervous before participating and had a lot of self doubt about taking part in this. I am so glad I did it! I played the drums (my first choice of the 3 instruments I put on my paperwork) at Ladies Rock Camp and this was the first time I had seriously played since I was 17 years old. I had a bad experience with a band director in high school and was picked on for being one of the only girls (and good) who played the drums in middle school and thought that I would never play again. This experience was amazing and really boosted my self confidence. I feel like I was able to reconnect with this part of my 17 year old self and it felt really healing. It was nice to prove to myself that I could do something that felt really scary and out of my comfort zone and actually excel at it. I didn’t even get mad at myself when I goofed up during our performance (big deal for me!). This is something I try to hold on to when I am having difficult moments and I am slowly starting to add the drums back into my life as a fun activity. This was definitely one of the heights of the rollercoaster of the past year.
Part of the reason why I am writing about all of this now because not only do I need to sort out the thoughts in my head, but I think I need to reach out for help from my friends and family. Writing seems to be the only way in which I am able to articulate my thoughts and needs in an effective way.
I was diagnosed with stage 4 endometriosis after having surgery on 08/01/2018. The doctor who diagnosed me was the 7th doctor I had seen for the chronic pain I had been experiencing at that point for two years. Although that surgery relieved a lot of my pain, I started having chronic back pain again in October of 2018. Since then my pain has increased and is now affecting different parts of my body. Currently, and in the past 6 months, my pain levels radiate between 6 out of 10 to as bad as 10 out of 10 on the pain scale. My wife tells me I am not an effusive or demonstrative person (What?! who is surprised by that other than me?!) and that she has not been aware that I have been in that much pain since I don’t go into detail when I tell her I am hurting. To me, saying that, “I am hurting” means that I am in a lot of pain because I don’t usually complain. I think that I am conveying to people how I feel when apparently I am not getting my point across. That has been a big source of frustration in general for me, as I think I am communicating to people when I am actually not. I need to keep this in mind and try to be more descriptive with my words.
After almost 8 months of physical therapy ($$$ because hardly any pelvic floor therapists in Georgia are in network with insurance), an MRI, a back x-ray, appointments with my primary care physician, my surgeon and a rheumatologist, I still did not really have any answers about why I was continuing to have chronic back, hip, glute, thigh and heel pain. In early April, I became a little desperate about my increased pain and decided to get a 2nd or 8th (depending on how you look at it) opinion from a doctor in Chattanooga who was in network with my insurance and really seemed to know his stuff. When I called the earliest appointment he had available was 08/06/2019, so I went ahead and scheduled it.
On my birthday, 4/30/2019, the surgeon who originally diagnosed me, called me to let me know I had some concerning cysts and “fluffy” tissue that her radiologist noticed on the MRI I had in February (after Emory told me it was normal- the 2nd MRI they have misread). She let me know that she would need to do multiple procedures along with a biopsy as soon as possible to determine if that was causing my recurrence of pain and to rule “other things out.” Of course I immediately went into panic mode and consulted Dr. Google! Bad idea… My immediate concern became that I might have cancer. I continued to pretty much obsess about this until we finally got the results of my biopsy. Almost two months after that phone call and the procedures, I found out that I did not have cancer and that the “fluffy” tissue was likely due to the excess estrogen that is caused by endometriosis. Not a definitive answer as to if this is causing my pain. My doctor seemed pretty unconcerned with my pain levels, especially since my test results all came back “normal.” I decided to keep that appointment with the other doctor in Chattanooga in hopes that he might have some insight.
I am really glad I kept the appointment with the surgeon in Chattanooga. He listened and asked questions in a way no other doctors had up until that point. He knew from looking at my previous surgery pictures that I still had endometriosis on my intestines and most likely in other areas in my abdominal area. He told Leah and I that I would need another surgery and explained that I would need to have my appendix removed because it can be a pelvic pain generator and excise any endometriosis that he finds when he goes in. He also highly recommended that I get a hysterectomy and he will leave it up to me as to whether I keep my ovaries or not. He did extensive blood work at that appointment, ordered a lumbar MRI (in hopes to see if he could tell what was causing my back pain, although he is pretty sure it is endometriosis). I left that appointment in tears- partly because the drive to Chattanooga felt amazing compared to Orlando (my other surgeon’s office is there) and really because, once again I know my body best and I am not crazy. He validated the fact that I knew and still know that there is something wrong with my body and my surgery was scheduled by the time I left his office. His office is so much more efficient than my previous surgeon. He answered all of my and Leah’s questions in detail and spent over an hour with us at my appointment.
I thought that waiting 4 months for my appointment with him would probably be the most difficult thing out of this process, well I was wrong. Our insurance changed in July of 2019 and I have been trying to get the MRI that my doctor ordered approved by our insurance company for two months at this point. My doctor’s office and I have spent hours on the phone with them, he did a peer to peer review (where your doctor tries to convince one of the insurance company’s doctors that you need whatever procedure they’re denying), and I wrote an appeal letter- including my eight months of physical therapy notes, my x-ray results, and a note from my therapist (basically saying that chronic pain and constant self-advocacy and battles with insurance is affecting my mental health). I am still in limbo as of today as to whether they will cover my MRI and my surgery date is 20 days away. I thought that having three months in between my appointment and my surgery date would give me plenty of time to get everything in order. As of today, I still don’t know if they are going to approve my surgery that is scheduled out of state in less than 3 weeks.
Everything came to a head last night and I had an epic meltdown. I started crying while I was cooking because we were out of avocado and that was supposed to go into the meal that I was cooking. I am on a crazy anti inflammatory/endometriosis/ interstitial cystitis diet to try to manage my pain and inflammations and it was the avocado that tipped me over the edge! All the feelings that I have been keeping at bay by remaining constantly busy, productive, researching and planning, all came rushing to the surface and finally I let myself stay with my feelings and allow them to move through me. I am so so tired. Being in constant pain and remaining a productive member of my household, job, and society in general is so draining. I am very careful as to how much we have scheduled outside of work because even a fun and easy dinner with friends is exhausting. I know that I have been isolating myself for this reason and also having a chronic illness that involves my lady parts is not necessarily the easiest thing to talk about, nor the most acceptable in our society. I am aware that I am not reaching out to people when I need to and I am going to work on this.
It’s very hard to try to process losing my uterus when I don’t even know if or when it is actually going to happen. It feels hopeless to have to fight with my insurance company when I am in so much pain and the dark thoughts I try to keep at bay come bubbling up to the surface. These suicidal thoughts make me feel riddled with shame along with the shame that comes with having endometriosis in the first place. Not to mention having to prove to doctors and insurance companies that there is something wrong with my body. This is something that needs to be discussed. 1 in 10 women have endometriosis and so many women have hysterectomies and don’t talk about it. I would love any input from those who have had one, as to what to expect, tips and anything else I might need to know.
I am scared about my surgery. I am scared that the surgery won’t help and that I will feel this way the rest of my life. I am scared of not knowing how long I will be out of work (it will depend on exactly what is done in surgery and we won’t know until it happens). I am terrified that we will have to go into debt or that I will have to delay this surgery even longer. I am scared that permanent damage is being done to my body while I am in this limbo. I worry about Leah having to take on most of the household responsibilities while I am recovering, and the toll her worry over me takes on her. I worry that I made the wrong decision in not having kids now that it is almost too late. I worry about possible complications from my upcoming surgery. I am so anxious about our insurance and whether we will have surprise bills IF they even approve my surgery.
Did you know?
- Endometriosis is one of the top three causes of female infertility
- An estimated 8.5-10 million women in the US and 200 million (that’s 200,000,000) worldwide are believed to be affected
- Extremely painful menstruation, endometriosis’ most commonly known symptom, is the leading cause of missed work and school in young girls and women, according to one NIH study
- Endometriosis commonly goes undiagnosed or misdiagnosed, with women experiencing about 6-10 years delay before being correctly diagnosed
- Endometriosis is also frequently undiagnosed in teenage girls, due to persistent medical myths, like the false belief that pain with periods is normal or that teenagers rarely get endometriosis
Taken from http://nezhat.org/endometriosis-treatment/endometriosis/